The world-renowned Scientific Advisory Board (SAB) of physician-scientists only chooses the best and brightest emerging arthritis research scientists each and every year. Donor support of these scientists and the research they are doing is critical to discovering new therapies and treatments, and creating a path to a cure for arthritis and related autoimmune diseases. In addition, when a scientist receives funding, it propels the ability to establish their independent research careers. Ensuring they stay in research and spend their lifetime dedicated to finding a cure will translate into a commitment to the research needed to make an impact.
Ninety-five percent of ANRF funded scientists remain in research working towards a cure. These individuals work in top laboratories and ANRF funding enables them to make discoveries more quickly than without the extra support. The time is now to find a cure and help those suffering with arthritis.

“The Role of Neutrophils and NETs in the Pathogenesis of Scleroderma”


“Activation and Repertoire of Autoreactive B cells in Systemic Lupus Erythematosus”

“Defining the Role of UBA1 in Autoimmune Disease”
Gale “Morrie” Granger Fellowship
“Virus-induced Predisposition to Lupus after TLR7 Stimulation”
Carl F. Ware Fellowship

“An Articular Cartilage Stem Cell Mediating Cartilage Regeneration for The Treatment of Osteoarthritis”

“The Role of Cytokines in Monocytes During Macrophage Activation Syndrome”

“Inflammatory Mediators of Synovial Resident Memory T Cell Formation”
Sontag Foundation Fellow


“The Role of Neuroimmune Metabolic Crosstalk in the Onset and Progression of Pain in Osteoarthritis”

“Adipose Tissue as a Memory T Cell Storage Site in Inflammatory Arthritis”

“A Non-Coding Genetic Risk Variant That Controls T-Reg Abundance”


“Identification of Self-Reactive T Cell Antigens in Systemic Sclerosis”

“Mechanisms of Th1.17 Cell Development in Polyarticular Juvenile Idiopathic Arthritis”
Staci Stringer Valiant Women Fellow

“Role of A20 in Restricting Psoriatic Skin and Joint Disease”
Janssen Immunology Psoriatic Arthritis Fellow
“Deciphering Complement-Dependent Phagocytic Myeloid Phenotypes in Human Autoimmune Arthritis Using Single-Cell Computational Omics”

“The Role of Neutrophils and NETs in the Pathogenesis of Scleroderma”
“Elucidating the Role of miR-126-3p in Osteoarthritis”

“Removal of Apoptotic Cells in Inflammatory Arthritis”

Synthetically regulated cell-based therapeutics for targeted articular cartilage regenerative medicine

“The Role of Cytokines in Monocytes During Macrophage Activation Syndrome”
“Epigenetic Mechanisms of Macrophages during Gouty Inflammation”

Platelets as neutrophil amplifiers in systemic sclerosis

“Adipose Tissue as a Memory T Cell Storage Site in Inflammatory Arthritis”

Splicing Disruption in Systemic Lupus Erythematosus
mTORC1 in the pathogenesis of systemic juvenile idiopathic arthritis

Understanding how the CARD9-neutrophil-Th17 axis controls ankylosing spondylitis
Mechanistic Insights into Organ-Specific Manifestations of Spondyloarthritis

“Mechanisms of Th1.17 Cell Development in Polyarticular Juvenile Idiopathic Arthritis”

“Role of A20 in Restricting Psoriatic Skin and Joint Disease”

Microparticle-assisted modulation of regulatory T cells in rheumatoid arthritis

Molecular reprogramming of Rheumatoid arthritis synovial fibroblasts by interleukin 6

Type I Interferon Pathway Activity Informs TNF-inhibitor Treatment Response in Rheumatoid Arthritis

Metabolic regulation of chondrocytes by Sirt5 and protein malonylation in osteoarthritis development

Mechanisms of infection-induced autoimmunity in COVID-19 and beyond

Characterize the role of AIM2 in the autoimmune disease Systemic Lupus

Synthetically regulated cell-based therapeutics for targeted articular cartilage regenerative medicine

Platelets as neutrophil amplifiers in systemic sclerosis

Splicing Disruption in Systemic Lupus Erythematosus

The Function & Autoreactivity of Th1 Polarized & Clonally Expanded Tregs in Oligo JIA

Analysis of the NOD-RIPK2 signaling pathway in osteoarthritis

mTORC1 in the pathogenesis of systemic juvenile idiopathic arthritis

Mechanisms by which clonal hematopoiesis augments inflammation and atherosclerosis in rheumatoid arthritis

Understanding how the CARD9-neutrophil-Th17 axis controls ankylosing spondylitis

Elucidating mechanisms of methotrexate metabolism by the human microbiome in rheumatoid arthritis
Mechanistic Insights into Organ-Specific Manifestations of Spondyloarthritis

The role of TNF and TNFR1 in breaking B cell tolerance

Microparticle-assisted modulation of regulatory T cells in rheumatoid arthritis

Molecular reprogramming of Rheumatoid arthritis synovial fibroblasts by interleukin 6
Immune Checkpoint Inhibition Induced Inflammatory Arthritis Correlates with Imbalance Between T-cell Exhaustion and Senescence
Investigating the role of gene Creb5 in lubricin expression during the development of osteoarthritis

Metabolic regulation of chondrocytes by Sirt5 and protein malonylation in osteoarthritis development

Mechanisms of infection-induced autoimmunity in COVID-19 and beyond

Characterize the role of AIM2 in the autoimmune disease Systemic Lupus
Investigating the role of resident stem cell populations in the regeneration of cartilage and in OA progression

Identifying why some children outgrow JIA whereas others develop chronic disease.
Investigate how such OCs form and how they lead to joint tissue destruction in arthritis.

Hypothesizes that mutations in specific genes as found in OA susceptible families may underlie the enhanced joint inflammation that is a hallmark of OA progression.

Evaluating the impact of mutations in the gene TET2 in RA since her previous work demonstrated that such mutations result in accelerated CVD development.

Characterize the microbiomes and Methotrexate (MTX) metabolites of a number of RA patients to more fully understand how specific bacterial genes may influence the activity of MTX in RA patients.

Investigating how TNF affects the generation of autoreactive B cells.

Understand how this specific DNASE1L3 polymorphism leads to the development of scleroderma

The genetics of antinuclear antibodies and the risk of lupus
Analyze ICI patient samples to determine the mechanisms that lead to the development of this form of arthritis following ICI therapy.
Investigating the role of gene Creb5 in lubricin expression during the development of osteoarthritis
Decoding rheumatoid arthritis using a unique tool to identify arthritogenic T cells

A Chemical Niche to Regenerate and Rejuvenate Cartilage in Osteoarthritis
Megakaryocytes as neutrophil amplifiers in inflammatory arthritis

Identification of pathogenic lymphocytes in ankylosing spondylitis

Origins of synovial osteoclasts in inflammatory arthritis
Epigenetics at the intersection of trauma, aging, and osteoarthritis

Characterization of a CD8 T Cell Subset Enriched in Blood of Patients with Rheumatoid Arthritis
The influence of the surrogate light chain protein λ5 on bone health and arthritis in aging

Identification of inhibitory receptors involved in establishing the Lyn-SHP-1 axis in B cell tolerance

The genetics of antinuclear antibodies and the risk of lupus

Mitochondrial-mediated inflammation and autoimmunity in rheumatoid arthritis

Targeting Platelet-Derived Growth Factor Receptor-α (PDGFRα) in Rheumatoid Arthritis

Understanding a shared mechanism for genetic risk in childhood arthritis

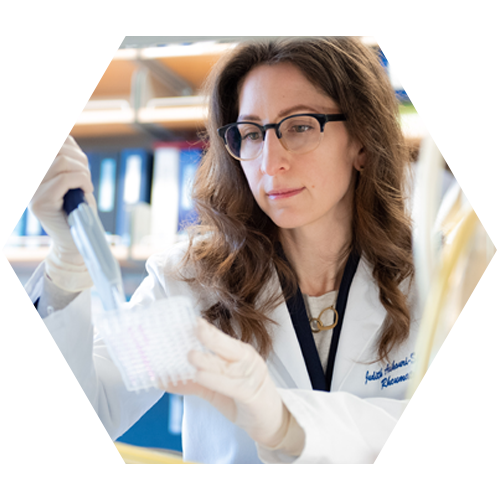
Sontag Foundation Fellow
Type I Interferon Pathway Activity Informs TNF-inhibitor Treatment Response in Rheumatoid Arthritis

Pathogenic effects of DNASE1L3 R206C polymorphism in systemic sclerosis

Derivation and phenotype of ANA+ plasma cells in SLE
Functional diversity of iNKT subsets in Rheumatoid Arthritis
Characterization of a novel epigenetic regulator of Th17 differentiation

Signaling and repertoire differences in arthritogenic T cells

Genetic reprogramming of OA chondrocytes to improve cartilage repair
Megakaryocytes as neutrophil amplifiers in inflammatory arthritis
Cellular senescence as a driver and therapeutic target for osteoarthritis
Epigenetics at the intersection of trauma, aging, and osteoarthritis

Characterization of a CD8 T Cell Subset Enriched in Blood of Patients with Rheumatoid Arthritis
The influence of the surrogate light chain protein λ5 on bone health and arthritis in aging

Role of IL36α in Osteoarthritis progression

Identifying Novel Mechanotransduction Targets for Treating Osteoarthritis

Targeting Platelet-Derived Growth Factor Receptor-α (PDGFRα) in Rheumatoid Arthritis

The Role of TNF and TNFR1 in Breaking B Cell Tolerance
The role of matricellular protein CYR61 in fibrosis and angiogenesis in scleroderma
Validating STAT3 as a Therapeutic Target in Arthritis
Characterization of a novel epigenetic regulator of Th17 differentiation
Comparing the Regulatory Networks Underlying Inflammation in Arthritis & Aging
The function of SENP6 desumoylase in preventing articular chondrocyte senescence and osteoarthritis development
Cells for Regenerating Articular Cartilage

Cellular senescence as a driver and therapeutic target for osteoarthritis
Mechanisms Underlying TACI-dependent activation of immature transitional B cells in BAFF-driven humoral autoimmunity

Therapeutic targeting of GPCR Gbetagamma-GRK2 signaling in osteoarthritis
Thrombo-inflammatory role of neutrophils in lupus
Activin A regulation of T follicular helper cell biology in Rheumatoid Arthritis

Identifying Novel Mechanotransduction Targets for Treating Osteoarthritis
Predicting tissue growth potential using high-throughput screening for cell mechanics
Genetic and Epigenetic Covariance of Gout, Hyperuricemia and its Comorbidities
Personalized approach to enhance prediction of psoriatic arthritis
The role of matricellular protein CYR61 in fibrosis and angiogenesis in scleroderma

Validating STAT3 as a Therapeutic Target in Arthritis

Comparing the Regulatory Networks Underlying Inflammation in Arthritis & Aging
Deborah R. Winter, PhD is the Sontag Foundation Fellow for 2017-2018.
The Intriguing Role of Macrophages in Rheumatoid Arthritis

The function of SENP6 desumoylase in preventing articular chondrocyte senescence and osteoarthritis development
Research: Rheumatoid Arthritis
Project Title: Identifying Cellular and Molecular Mechanisms of Microbiome-Driven Inflammatory Arthritis

Research: Psoriatic Arthritis
Understanding the Cause of Psoriatic Arthritis

Research: Osteoarthritis
Cells for Regenerating Articular Cartilage

Research: Osteoarthritis
Elucidating the function of musculoskeletal promoting small molecules for osteoarthritis
Research: Lupus
Mechanisms underlying TACI-dependent activation of immature transitional B cells in BAFF-driven Systemic Lupus Erythematosus (SLE)
Research: Lupus
Thrombo-inflammatory role of neutrophils in lupus
Research: Adult and Pediatric Rheumatoid Arthritis
High-throughput experimental interrogation of GWAS loci in adult and pediatric arthritis
Research: Gout
Genetic and Epigenetic Covariance of Gout, Hyperuricemia and its Comorbidities

Research: Autoimmunity
Role of the transcription factor Ikaros in development of autoimmune disease
Research: Autoimmunity
The innate immune adaptor STING regulates age-dependent bone homeostasis and remodeling.

Research: Rheumatoid Arthritis
Unraveling a novel mechanism of action of PTPN22, a major RA gene

Research: Psoriatic Arthritis
Personalized approach to enhance prediction of psoriatic arthritis

Research: Lupus
Regulation of Treg metabolism and stability by PTEN in autoimmune diseases

Microbiome-Driven Inflammatory Arthritis: Studying Bacteria as Cause of RA

How Joint-Protecting Cells Transform into Joint-Destroying Cells

Osteoarthritis (OA) study could lead to new treatment

Genetic Mechanisms in Inflammatory Arthritis
Understanding the Cause of Psoriatic Arthritis
Co-Funded Grant with National Psoriasis Foundation

Study to prevent or reverse damaged Osteoarthritis joints

Skin Rash Triggers Kidney Inflammation

Gene Study may provide targeted treatment for RA, JIA patients

Inherited Immune Cell Defects May Hold Key to Understanding

Gene could provide key to understanding autoimmunity
Understanding initiation of bone loss may yield new targets for treatment

Genetic study may lead to targeted treatment
Laying a foundation for new OA therapy

Damage in joints of patients with rheumatoid arthritis (RA) is induced by the patient’s immune system attacking its own joint tissues. However, a portion of this damage is caused by “resident” normal cells in the joint that have become altered during and after the immune attack. The altered resident cells undergo abnormal growth and healing which results in scarring, disfigurement and joint immobilization.
Studying joint tissue from human RA patients and mice, Dr. Bartok has discovered how the normal joint cells become altered by the immune attack. Her important findings can lead to the development of new methods to block this destructive cellular response. This can lead to new drugs and treatments to prevent and stop the progressive destruction of joint tissues in RA patients.

Rheumatoid arthritis is a common joint disease causing distress and disability in the affected individuals. Abnormal changes in specialized cells lining the joint surfaces, known as the fibroblasts-like synoviocytes, are one of the major causes of this disease. In healthy joints fibroblasts-like synoviocytes are critical for the maintenance of joint integrity. They produce molecules that lubricate joints and help to protect joints from wear and tear. However, in rheumatoid arthritis, these specialized cells transform into cancer-like cells. They increase in numbers and act as a source of molecules that destroy the joints.
Despite this knowledge, incomplete understanding of the genes and pathways that regulate fibroblasts-like synoviocytes has limited the development of treatment strategies that can target these cells. This study focuses on uncovering the roles of a group of genes that belong to the SOX family, in transforming the healthy joint protecting cells into joint destroying cells. The signaling pathways that are under the control of these SOX genes could be targeted to treat and limit the joint damage in rheumatoid arthritis.

Osteoarthritis is the most common form of arthritis that affects approximately 27 million people in U.S. alone. Current treatments are however limited to pain management mainly because of a lack of understanding of the initiation and early stages of the disease. No disease-modifying OA drug is available as a result. OA is marked by joint dysfunction and particularly cartilage degeneration caused by the native cartilage cells themselves. Dr. Bhutani’s recent studies have identified that normal and OA cartilage cells from patients differ greatly in the function of a novel family of enzymes. These enzymes are responsible for modifying the DNA and such ‘epigenetic’ modifications affect widespread gene expression; therefore, these enzymes can be central regulators of the gene expression changes in OA.
Dr. Bhutani’s research will identify the genes that are regulated by these particular enzymes in OA cartilage to understand how they affect the initiation and progression of OA. Using mice that lack these enzymes, she will test how the absence of this regulator will modulate OA. Lastly, Dr. Bhutani will evaluate whether a pharmacological manipulation of these enzymes (and its targets) has the potential to be therapeutic in OA.
Dr. Bhutani is the ANRF-AFAR Grant Recipient – a special grant on aging co-funded by ANRF and the American Federation for Aging Research.

While acute inflammation is mostly beneficial, unchecked or dysregulated inflammation can have devastating consequences leading to a wide range of diseases including Rheumatoid Arthritis, Systemic Lupus Erythematous, and Cancer. Thus, given the significance of these devastating diseases, new approaches towards understanding pathology and gene mechanism are urgently needed.
It has been over a decade since the human genome was sequenced. Since then, there have been huge improvements in our ability to carry out sequencing. The classical understanding of the genome was that DNA is transcribed into RNA, which makes proteins that carry out various biological functions. However, sequencing studies have shown that only a small portion (2%) of the genome results in protein, yet there are very large amounts of RNA being produced (85% of the genome). The major class of RNA molecules produced from the genome are called long noncoding RNA (lncRNA). These RNA molecules are emerging as fundamental mediators of innate immune signaling pathways.
Dr. Carpenter’s research has identified lincRNA-Cox2 as a highly inducible gene in response to inflammatory stimuli and functions to repress interferon stimulated gene (ISG) expression while also being required for the induction of other inflammatory genes such as IL-6. She has identified functional interactions between lincRNA-Cox2 and the heterogeneous nuclear ribonucleoprotein A2/B1 (hnRNP-A2/B1), also known as RA33, an auto-antigen in rheumatoid arthritis.
This project aims to understand how lincRNA-Cox2 and RA33 are involved in the pathogenesis of inflammatory arthritis. Obtaining a better understanding of the role of these RNA molecules in inflammatory conditions could lead to the development of new biomarkers for disease and unveil new therapeutic targets.
Articular cartilage is a type of connective tissue that covers the surfaces of bones within synovial joints. Articular cartilage injury and the lack of cartilage regeneration often lead to osteoarthritis. Recent studies carried out by Dr. Evseenko and his lab and others have shown that stem/progenitor cells can partially repair damage cartilage, but more work is needed to increase the efficiency of this therapy. Unfortunately, limited survival and degeneration of implanted stem/progenitor cells, as well as excessive collagen type I (COL I) deposition leading to formation of mechanically inferior tissue, are the standard outcomes of currently used cell-based cartilage restoration techniques.
Dr. Evseenko proposes a novel approach based on his recent findings and the development of an essential model to test this and subsequent therapeutic methods. He will use a highly purified population of cartilage stem cells identified in his lab’s recent studies of normal human cartilage development. His team will also manipulate signaling driven by the small biogenic lipid LPA, having recently shown that LPA is highly expressed in the site of cartilage injury driving COL I deposition, which in turn leads to fibrosis and limits the expansion and survival of implanted stem cells. In rat studies, his team has also shown that pharmacological inhibition of the LPA-signaling reduces fibrosis and results in enhanced production of neocartilage at the site of injury.
During this second year of ANRF support, Dr. Evseenko will access this novel approach in a large animal model of joint injury and apply a highly innovative robotic approach to assess the biomechanical properties of repaired joints, in addition to the routine histological tests. The ultimate objective of the proposed project is to develop new therapeutic approaches for articular cartilage restoration, which in turn will reduce the morbidity from acute cartilage injuries and degenerative joint disease.
Dr. Evseenko is this year’s James Klinenberg Scholar as his work at UCLA closely aligns with that of Dr. Klinenberg.

Systemic lupus erythematosus (SLE or lupus) is a severe autoimmune disorder that can adversely affect many organs, including the skin, kidney, blood and joints. This organ damage can result in substantial morbidity or even death. In patients suffering from lupus, their disease course is characterized by “flares” of increased disease activity that require treatment with aggressive immunosuppressive medications. Often, these flares can be heralded by the presence of a lupus rash. However, how this rash relates to systemic disease development remains unclear.
In most murine models of lupus, the onset of disease is a gradual process, and it has been difficult to model how a flare occurs. In her work, Dr. Kahlenberg has developed a model in which lupus-prone female mice develop a rapid flare of kidney disease following skin injury. This project proposes to determine the mechanisms by which skin injury can lead to a rapid flare of kidney inflammation in these mice. She will investigate this by undertaking a systematic exploration of the inflammatory cell populations present in the kidney and relate this to simultaneous changes in the skin and blood of the mice. Additionally, she and her team will target the cytokine IL-18 to determine whether induction of flares of kidney inflammation by skin injury requires this cytokine.
She anticipates this work will show that skin injury rapidly increases the inflammatory cell populations in the kidney and that blocking IL-18 may modulate this. This work will benefit the scientific community by increasing knowledge of how the skin and kidney may cross-talk in lupus, thus leading to development of novel therapies that may help to prevent flares of lupus nephritis and reduce the need for immunosuppressive medications in lupus patients.
Dr. Evseenko is this year’s Eng Tan Scholar as her work most closely aligns with that of Dr. Tan.

Rheumatoid arthritis (RA) affects 0.5-1% of the general population and is characterized by joint inflammation (arthritis) and increased mortality, primarily due to heart attack and stroke. Scientific breakthroughs during the last 20 years have enriched our therapeutic “medicine chest” with biologic therapies and kinase inhibitors, leading to a dramatic improvement in patients’ quality of life. Despite this progress there are still unmet needs including the low rates of sustained disease remission and the inadequate response to therapy in about 1/3 of RA patients. In this context, it is necessary to implement more individualized treatment protocols and identify safer and more effective therapies. The path to achieve these goals is to understand in depth the molecular events implicated in RA pathogensis.
Dr. Kalliolias uses novel technologies to characterize the role of synovial fibroblasts (SF) in RA pathogenesis. SF are resident cells of the normal joint that become activated in RA. Although their implication in the inflammatory and destructive processes of RA has been considered for a long time, none of the existing therapies for RA targets SF. His previous studies have shown that SF display an uncontrolled inflammatory response to factors found in abundance within the inflamed joint of RA patients. These findings led to the hypothesis that SF of RA patients lack the appropriate “brakes” that should turn off inflammatory responses. Currently, Dr. Kalliolias is testing this hypothesis with an ultimate goal to identify strategies to terminate or block the production of inflammatory and tissue destructive mediators by SF. His long-term goal is to set the stage for the development of drugs for RA patients that will target SF, supplementing the existing therapies that target the immune system.
Dr. Kalliolias was named the first Gale A. Granger Scholar, as his work most closely aligned with that of Dr. Granger, former ANRF grant recipient and board member who initially discovered tumor necrosis factor (TNF) and its receptors.

Antiphospholipid syndrome (APS) is a serious autoimmune clotting disorder in which the immune system mistakenly attacks a self-protein in the blood. The “auto antibodies” that attack self molecules in blood are found in certain patients with rheumatoid arthritis, lupus and other autoimmune diseases. When the auto antibodies react with self molecules they form clots in the blood stream that can lodge in tissues causing stroke, heart attack and death. What induces the patient’s immune system to react against these self molecules is not known.
Dr. Kriegel has found that certain bacteria living in the digestive tract of patients with APS trick the immune system to react against the self molecules. These are important findings for they reveal 1) how this disease starts which may serve as a model of how other types of autoimmune disease can start and, 2) how to diagnose, prevent and stop the progression of this particular disease.

Nutrition can have a profound effect on disease development. Most current studies have focused on how macro-nutrition (calorie, carbohydrate, fat, and protein) affects diseases, but very little is known about the role that early life micro-nutrition plays in diseases such as rheumatoid arthritis (RA). Micronutrients such as folic acid and methionine produce methyl donors that can attach to DNA. The amount of protein produced by a gene can be increased or decreased by the amount of methyl donors attached to that gene’s DNA. When this happens, the gene is considered “methylation sensitive.”
Tissue damage in rheumatoid arthritis is caused by certain pro-inflammatory genes, and many of these genes are methylation sensitive. A subset of white blood cells, CD4+ T cells, contributes to RA by producing high levels of many pro-inflammatory proteins, and disease severity can be adjusted by controlling the methylation level of several of these genes. Feeding mice a diet rich in methyl donors during pregnancy affects expression of many of these genes in CD4+ T cells in their offspring mice (F1 methyl supplemented), compared to the offspring of pregnant mice that were fed a regular diet (F1 control). Genes favoring inflammation are expressed at lower levels in F1 methyl supplemented mice and, in a model of atherosclerosis (heart disease), F1 methyl supplemented mice had less severe disease than F1 control mice.
Dr. Patel predicts F1 methyl supplemented mice will have less severe rheumatoid arthritis, compared to F1 control mice, as well. His team has shown, in the collagen induced arthritis model, F1 methyl supplemented mice have decreased paw swelling compared to F1 control mice. To explain this, he expects that CD4+ T cells will express lower levels of pro-inflammatory mediators, and higher levels of anti-inflammatory mediators, in F1 methyl supplemented mice compared to F1 control mice.
These results have the potential to transform our understanding of how genes and the environment interact in RA and other chronic inflammatory diseases, and to identify a new paradigm in understanding and potentially treating inflammation and disease with pre-natal nutrition.

Neutrophils are white blood cells which are important for the body’s defense against infectious agents. However, these same cells enter the joint in rheumatoid arthritis in large numbers and over time cause swelling, pain and tissue damage.
Dr. Wang has identified the mechanism of how neutrophils leave the blood stream and migrate into joint tissues. These are important findings for blocking the migration of neutrophils into the joint can prevent the onset of the disease and stop tissue damage. These results can lead to new methods to prevent and control RA and other forms of inflammatory arthritis.
Current osteoarthritis (OA) treatment focuses on symptom relief but does not materially alter disease progression. OA prevention and treatment continue to be a clinical challenge due to the limited self-healing capacity of joint cartilage. Searching for cell sources capable of being mobilized and providing functional descendants in joint cartilage is of paramount importance to osteoarthritis prevention and treatment.
Dr. Yang and his team recently identified a population of cartilage progenitors/stem cells that express an enzyme called cathepsin K in joints; these cells are capable of forming cartilage and this function is enhanced in the absence of a certain protein, tyrosine phosphatase SHP2. The goal of this study is to further understand the role of this population of stem cells in joint cartilage development and homeostasis and the molecular mechanism through which this protein modulates the capability of the stem cells to form cartilage. Dr. Yang’s long-term objective is to develop strategies to inhibit cartilage degeneration and promote its regeneration by mobilizing this population of stem cells and/or modifying SHP2-regulated signaling pathway(s).

Systemic lupus erythematosus (SLE or lupus) is an autoimmune disease in which the immune system turns against parts of the body it is designed to protect. With lupus, instead of producing protective antibodies, the immune system makes autoantibodies, which attack the patient’s own tissues and cause widespread tissue and organ injury. These autoantibodies are secreted by large number of plasma cells, which are differentiated from a type of leukocytes (white blood cells) called B cells, and are heavily mutated on the antigen-binding domain and class-switched to mainly IgG isotype.
The pathogenesis of autoimmune diseases, including lupus, can be traced to both genetic elements and epigenetic modifications arising from exposure to the environment. Epigenetics involves genetic control by factors other than an individual’s own DNA sequence. Epigenetic factors, such as DNA methylation, histone modifications and microRNAs, can switch genes on or off and determine which proteins impact cell function. Like many other autoimmune diseases, lupus preferentially affects women during their reproductive years, suggesting that the female hormone estrogen, which promotes autoantibody response, plays an important role in causing lupus.
In Dr. Zan’s study, he and his team utilizes FDA-approved and widely-used epigenetic modulators to selectively inhibit the generation of pathogenic autoantibodies to prevent, treat or even cure lupus. With the second year support from Arthritis National Research Foundation, he will develop therapeutic approaches including combined treatment that target both estrogen receptor, which is important for effects of estrogen, and epigenetic factors, or target multiple epigenetic factors to synergistically dampen autoantibody responses, thereby, treat lupus more effectively. He will also attempt to gain further insight into B cell-intrinsic epigenetic mechanisms in the pathogenic lupus autoantibody response, and to unveil modulation of the epigenetic factors by estrogen.

Rheumatoid arthritis is a chronic, debilitating condition that affects about 1% of the population in U.S. Chronic inflammation leads to joint destruction, loss of function, and severe disability in addition to shortened life expectancy, most commonly as a result of accelerated heart disease. Despite the major breakthrough with the introduction of biologics, treatment of rheumatoid arthritis remains an unmet medical need. These costly therapies have not been effective in all patients nor have they shown long lasting benefit after discontinuation.
Fibroblast-like synoviocytes are resident cells of the joints that play a critical role in rheumatoid arthritis by participating in inflammation and joint destruction in concert with the cells of the immune system. Therefore, therapies that specifically target these cells are highly desirable and have the potential to halt disease progression and even be curative. The proposal focuses on the investigation of a novel protein called YAP and signaling pathway that is dysregulated in rheumatoid arthritis and might be responsible for synoviocytes’ mediated joint destruction and inflammation. Reprogramming fibroblast-like synoviocytes by modulating the YAP pathway can lead to novel and effective therapy for patients with rheumatoid arthritis.

Macrophage Activation Syndrome (MAS) is a life-threatening complication of a number of rheumatic illnesses, particularly systemic juvenile idiopathic arthritis. It manifests as the rapid onset of severe systemic inflammation. Currently, our understanding of the causes, risk factors, diagnosis, and treatment of MAS remains very poor. Initial investigations have implicated abnormal signaling through Toll-like Receptors (TLRs) or dysregulated function of the anti-inflammatory cytokine Interleukin 10.
Using clues from patients and model systems, Dr. Canna aims to understand how such defects contribute to MAS. Dr. Canna is the recipient of The Kelly Award for Juvenile Arthritis Research for 2013.

Posttraumatic cartilage injury is one of the most significant problems among orthopaedic surgery patients. There is strong evidence that cartilage lesions predispose to osteoarthritis when left untreated. Osteoarthritis is a group of mechanical abnormalities involving degradation of joints, including articular cartilage and bone. OA is the most common type of arthritis.
Different cell types have been studied with respect to their ability to generate articular cartilage. Unfortunately, cartilage tissue derived from these populations represents functionally inferior fibrocartilage, characterized by massive and disorganized collagen 1 deposition while normal hyaline articular cartilage predominantly contains collagen type 2. Dr. Evseenko’s study identifies a novel potential regulator – lysophoshatidic acid (LPA) — that can play a mechanistic role in the process of fibrocartilage formation.
The overall goal of this work is to determine if modulation of the LPA signaling can be used to direct stem cell differentiation, so that cartilage defects are repaired with hyaline articular cartilage rather than fibrocartilage preventing progression of osteoarthritis.
Lupus is a chronic autoimmune disease driven by the production of autoantibodies. Our understanding of the mechanism(s) that drive autoantibody production in lupus remains poorly defined.
Dr. Gauld’s research group has discovered that a population of cells, called regulatory T cells (or Tregs), is essential to prevent autoantibody production. Tregs stop autoantibody production by preventing the expansion of a new, highly novel population of cells, called TAN cells. The goal of this project is to understand more about TAN cells. In particular, Dr Gauld’s research will investigate how TAN cells develop and how they instruct other cells to make autoantibodies. Achieving these goals could help identify new therapeutic targets for the treatment of lupus.
A more effective therapy for RA could be developed if the targeting of cells studied by Dr. Huang is successful. Rheumatoid arthritis (RA) and its mouse model, collagen-induced arthritis (CIA), are characterized by systemic and synovial tissue inflammation, beginning in the joints.
TH17 cells play a key role in the pathogenesis of arthritis. In this study, Dr. Huang examines the roles and mechanisms of p38α signaling in TH17 cell differentiation and function and the progression of collagen-induced arthritis in mice. His study may show that selectively targeting these cells would improve the efficiency of current treatments, and the use of novel drug-delivery vehicles to target the p38α inhibitors to specific tissue or cell types would be a promising strategy to avoid undesired side effects.

Because FoxA transcription factors play an important role in skeletal development, Dr. Ionescu has begun to explore whether this transcription factor family also plays a role during conditions such as osteoarthritis. So far, she has found that over-expression of the gene, FoxA2, in a murine model of osteoarthritis accelerates progression of the disease while deletion of this gene in osteoarthritis prevents disease progression and protects against cartilage degradation in the joints.
This raises the interesting possibility that the induced expression of FoxA transcription factors during osteoarthritis leads to cartilage degradation. Thus, FoxA2 may be an interesting target for small-molecule inhibition in hopes of preventing OA.

B cells are an important part of a normal immune system; however, their function is altered in patients suffering from many autoimmune diseases. Patients with rheumatoid arthritis have been shown to benefit from treatment targeting this cell population. BAFF is a crucial survival factor for B cells and BAFF serum levels have been shown to be elevated in patients suffering from different autoimmune disorders including rheumatoid arthritis. This project will study biochemical signaling pathways activated in B cells by BAFF and their contribution to B cell maturation and survival. A better understanding of these signaling pathways could lead to the development of new therapeutic agents or treatment strategies.

T cells that are activated by and react to the body’s own tissues are among the cells that drive autoimmune diseases such as rheumatoid arthritis (RA). Whether a T cell becomes fully activated is controlled by two mechanisms: 1) regulatory T cells inhibit T cell responses that are directed against the body’s own tissues and 2) so-called co-stimulatory and co-inhibitory molecules fine tune the T cell response and set the threshold for T cell activation. Among these, the co-inhibitory molecule TIGIT was recently linked to susceptibility to multiple autoimmune diseases, including RA. Dr. Joller’s study will determine how TIGIT regulates the autoimmune T cell responses that drive RA.
Dr. Joller will pursue an interdisciplinary approach to elucidate the inhibitory function of TIGIT. The knowledge gained through this approach will help Dr. Joller identify therapeutic targets and opens up different possibilities for the development of new therapeutic strategies.

Rheumatoid arthritis (RA) is characterized by chronic unremitting joint inflammation. Despite the progress in our understanding of RA pathogenesis, sustained disease remission is an unmet need for >50% of RA patients. The goal of this project is to identify novel therapeutic targets to stop efficiently and safely the damaging progress of RA.
Dr. Kalliolias hypothesizes that the new targets to block are fibroblast-like synoviocytes (FLS), critical players helping perpetuate joint inflammation. Approved therapies for RA target immune cells or their products primarily and, to date, there is no therapeutic strategy available to block the disease-causing functions of FLS.
Dr. Kalliolias anticipates these studies will set the stage for designing novel FLS-targeting therapies, enriching the existing therapies available without increasing immuno-suppression of RA patients.
The Sontag Foundation felt that Dr. Kalliolias and his innovative project were among the most promising of this year’s RA-related projects and named him The Sontag Fellow of the Arthritis National Research Foundation for 2013-14. Learn more about The Sontag Foundation’s commitment to rheumatoid arthritis research.

Osteoarthritis (OA) is the most common form of arthritis and current therapies primarily treat pain symptoms. The lack of a cure for OA clearly indicates that novel investigative approaches are needed to elucidate the functional changes occurring during this joint degenerative disease and to develop new therapies.
A joint is the location at which two or more bones connect and is surrounded by the joint capsule. The joint capsule is filled with a viscous fluid (synovial fluid) that protects the cartilage located at the surfaces of bones, called articular cartilage. In healthy joints, a proper joint structure is maintained by preventing the cells of the articular cartilage from undergoing mineralization followed by bone replacement, such as normally occurs during long bone growth.
If OA is the result of the failure of articular cells to establish the correct microenvironment and prevent joint mineralization, understanding the mechanism by which these cells preserve articular cartilage in adults can lead to understand how cartilage is damaged and to develop new treatments for OA.
Dr. Longobardi’s study is based on her original finding that the growth factor TGF-β (Transforming Growth factor-β), which is known to have a critical role in preserving the joint structure, can modulate joint development during fetal life by selectively repressing specific molecules secreted by inflammatory cells (cytokines), such as MCP-5 (Monocyte Chemoattractant protein-5). It has been proved that a correct balance between growth factors and cytokines is critical to maintain the properties of the articular cartilage.
The overall objective of the proposal is to analyze in more detail the mechanism by which TGF-β and MCP-5 interact and the molecules they activate to preserve joint integrity. This is a novel perspective to study OA disease progression in which joints are not the passive “victims” of the degenerative force of inflammation but rather make their own contribution to OA pathogenesis by the failure of an active cell joint population to maintain a controlled environment. The information derived from these studies has major medical relevance and implications as it will provide critical insights to the chain of events that lead to OA pointing the research toward novel therapies to restore joint function.

Rheumatoid arthritis (RA) is a chronic inflammatory disease that primarily affects joints leading to joint pain, stiffness, deformity and disability. Collagen induced arthritis (CIA) is a classic mouse model of RA which has substantially furthered our knowledge about the mechanism of the disease. Although RA is traditionally known as an autoimmune disease, innate immunity orchestrates the development of adaptive responses and pathogenic responses that drive RA. Targeting innate immune responses has proven beneficial in RA patients. Nucleotide binding and Oligomerization Domain (NOD)-like Receptors (NLRs) have recently emerged as important regulators of the innate immune response.
In this study, Dr. Malireddi will evaluate the role of NOD like receptor protein NLRP12 in the negative regulation of the immune response in rheumatoid arthritis using the CIA mouse model. This study could reveal the essential mechanisms of the innate immune responses required for suppressing inflammation and subsequently controlling arthritis causing factors. An understanding of such anti-inflammatory mechanism is a prerequisite for the development of new therapies.

Gout and pseudogout are chronic diseases caused by the precipitation in the joints of crystals of monosodium urate and calcium pyrophosphate dihydrate. Defining which cell types in the affected joints initiate and/or perpetuate the inflammatory response and related joint pathology induced by such crystals is an essential step towards finding more effective treatments.
Mast cells are potent pro-inflammatory immune cells which are abundant in the joints but their role in gout and pseudogout remains unknown. In this project, Dr. Reber will define mechanisms by which mast cells contribute to joint disease in mouse models of gout and pseudogout and assess whether and to what extent targeted inhibition of mast cell functions can reduce inflammation and disease pathology.

The neutrophil represents the front line of immune defense, migrating first into inflamed tissues to clear invading pathogens. However, in rheumatoid arthritis (RA) and other types of arthritis, neutrophil recruitment into the joints continues unabated for years, contributing to pain, joint swelling, and tissue destruction. Animal studies demonstrate that neutrophils serve a lynchpin role in both initiation and perpetuation of joint inflammation. Therefore, neutrophils are a potentially interesting therapeutic target.
The project will pursue the discovery of a novel regulator of human neutrophil migration, to understand how it works and to determine whether this protein could serve as a therapeutic target in inflammatory diseases such as arthritis.

Systemic lupus erythematosus (lupus) is an autoimmune disease characterized by the production of an array of pathogenic autoantibodies (antibodies that attack self tissues), which cause widespread tissue and organ injury.
Both genetic factors and epigenetic modifications that arise from exposure to the environment contribute to the pathogenesis of lupus. The word “epigenetic” literally means “in addition to changes in genetic sequence.” The term has evolved to include any process that alters gene activity without changing the DNA sequence, and leads to modifications that can be transmitted to daughter cells.
Dr. Zan’s research addresses core autoimmune mechanisms of lupus and will have sustained impact on the fields of epigenetics, immunoregulation and autoimmunity. This study will provide a sound mechanistic basis for use of inexpensive small molecule epigenetic inhibitors, some of which are already available and FDA-approved, to treat lupus more effectively.

Gout is the most common form of inflammatory arthritis and disproportionately affects adults over the age of 65; an estimated 4.7 million older adults have been diagnosed with gout in the US. There is increasing awareness that the risk factors, clinical presentation, and progression of gout differs for older adults.
To address the growing public health burden and distinct clinical aspects of gout in older adults, Dr. McAdams DeMarco’s research will estimate the number of older adults who develop gout, identify risk factors for gout in older adults, and determine the impact of gout on physical function in older adults. The findings from this research will lead to a better understanding of the burden, risk factors, and consequences of gout in older adults and will directly benefit patients and providers by characterizing this inflammatory arthritis in an understudied population.
Dr. McAdams DeMarco’s research is co-funded by ANRF and the American Federation for Aging Research (AFAR).
Charitable estate planning is financially beneficial for families and individuals of various ages and income levels, and ensures a legacy of commitment to making a difference through funding research, while supporting ANRF’s mission.

5319 University Dr #10022
Irvine, CA 92612
800.588.2873
Tax ID #: 95-6043953
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |